Our care is informed, compassionate and individualised
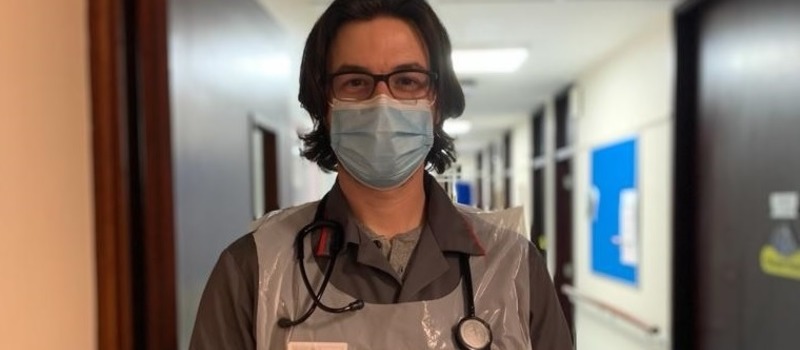
Dr Geoff Wells has been on placement at our hospice since October 2020. Here he shares his experiences.
“As a palliative medicine trainee, I’ve had the benefit of working in several hospices prior to joining St Catherine’s. I was excited to continue my training at St Catherine’s as it’s held in high regard amongst trainees who have trained here before me.
I started at the hospice during the coronavirus pandemic, and therefore things have been a little different on the inpatient unit as we adapt to the ever-changing situation.
Prior to joining St Catherine’s, I’d been completing a medical doctorate
I had already been seconded to work at the Royal Sussex County Hospital in the first wave of coronavirus in March/April 2020. This was a very unsettled time. Many junior doctors didn’t know where they may be working from one week to the next. Starting at St Catherine’s meant I regained some continuity and consistency at work. I didn’t have to worry that I may be sent off to a random ward at a moment’s notice. This also meant I could concentrate my efforts on my palliative care work, as well as an important palliative care exam that was due in November.
Early in the pandemic, as we learnt more about how COVID-19 spreads and affects people, I found the weekly changes in PPE guidance very confusing, I think we all did.
St Catherine’s has easily met my expectations
There are wonderful nursing, administration and therapies teams who work well together alongside the medical team. We have a very supportive consultant body and we’ve been lucky to have very enthusiastic and hardworking junior doctors who rotate every four months.
At St Catherine’s there’s a broad and varied skill mix which is a bonus for patients. We often find as doctors that we’re not always the most appropriate professionals to offer patients what they need. Instead it may be our nursing colleagues, therapies team or chaplaincy team who are much better placed to address specific individual needs.
Returning to training after three years out in academia was a little daunting
However, I’ve found the staff and my senior colleagues to be incredibly supportive. In particular I’ve noted that colleagues took the time to listen and get used to my way of working and thinking. They’re understanding that I won’t be as quick to step into the role of senior registrar straight away. Giving me space to get back into the swing of things and work out how St Catherine’s functions has been valuable for me as I look towards providing support to junior trainees now and in the future. I’m a strong believer that if your team are happy and feel respected, then this will permeate through to the care given to patients in a positive and meaningful way.
I feel privileged to be caring for individuals at one of the most vulnerable times in their life
I enjoy working alongside patients and relatives, and I feel privileged to be caring for individuals at one of the most vulnerable times in their life. That isn’t to say it isn’t challenging. All too often I find myself working with team members as we negotiate uncertainty in a patient’s illness, trying our best to help them make the right decision. Occasionally what a patient wants and what their family want aren’t the same thing. Working as a team we have to work through these challenges, providing facts, and keeping everybody as informed as possible to help them make difficult decisions.
Like many hospices, St Catherine’s offers patients time and space to work out what’s important to them, however long they have to live.
As much as we should be able to spend time with patients in any setting, this simply isn’t possible in a hospital setting where you may have 30 or 40 patients to look after. There aren’t enough hours in the day to be able to spend longer with patients there.
Many people think hospices are where you go to die -in fact the majority of our patients access our ward as an acute symptom control service
It’s important healthcare students undertake placements in a hospice because it will dispel any misconceptions they may have around the role and value of a hospice, and take away the fear and misinformation that still exists. Many people still think hospices are where you go to die. In fact the majority of our patients access our ward as an acute symptom control service. I think it’s also important for healthcare trainees to realise that we practice a decent amount of medicine, pharmacology, and need to have a good knowledge of physiology and anatomy in order to do our job well.
It’s important to train in different settings with different teams and patient groups, as this provides a broader wealth of experience than you’d get if you trained in the same place for a longer period. I’m able to learn from different ways of working and draw upon the skills and experience of consultants at St Catherine’s as I shape myself into a future consultant.
People will never know what the future holds for them
Illness has a habit of striking when we least expect it.
The hospice should be seen as a safe place rather than a sad place, it offers hope and support for people most in need. The large number of thank you letters demonstrate to us just how grateful people are for the services the hospice offers, and how positively different the hospice is to what they anticipated or assumed.
It’s often a better alternative to acute hospital care and will often enable patients to remain at home where they want to be, with their symptoms well controlled. Experts are on hand at the end of the phone 24 hours a day to offer expert advice.
Sadly, hospices only receive 30% funding from the government via the NHS, which means 70% must be found through charitable means. Without this funding hospices would no longer survive.”
If you would like to make a donation to help Geoff and his colleagues continue to provide expert care when it’s needed most please click here or call 01293 447361 – Thank you for anything you are able to give.